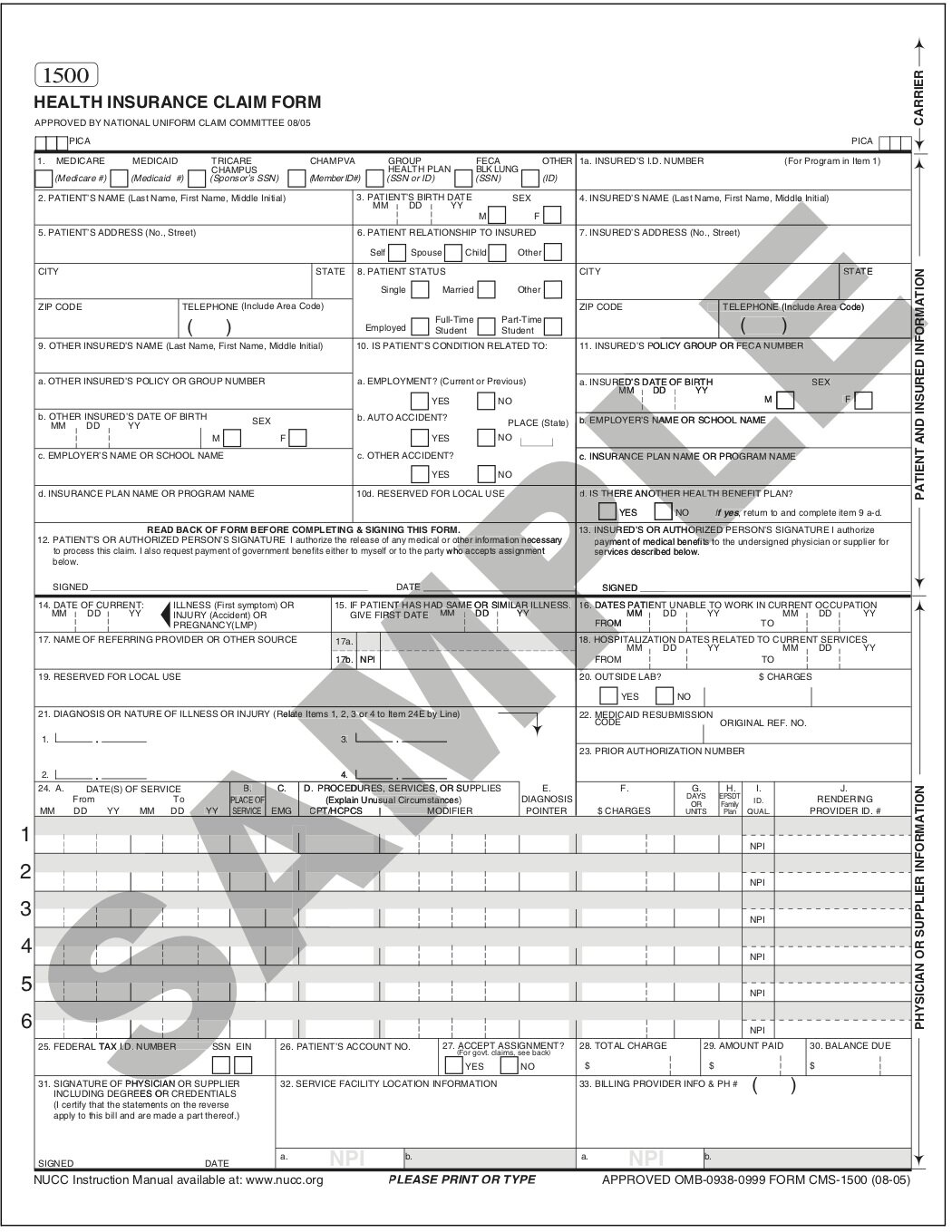
The Revised CMS-1500 Claim Form: Everything You Need to Know
History of the CMS-1500
In the 1960s many forms and coding systems were being utilized by third-party payers to provide information regarding services and procedures. There was a need for a standard paper claim form to be used by medical suppliers and physicians for claim billing. The American Medical Association (AMA), Centers for Medicare and Medicaid Services (CMS) and a group called the Uniform Claim Form Task Force collaborated to create the first iteration of the CMS-1500 Claim Form.
In 1990, the CMS-1500 changed the form to red ink print to promote the scanning of claims. Later, further changes were made in order to accommodate the National Provider Identifier (NPI).
To date, workers' compensation claims in NY (and a few other states) have utilized an alternate form in order to substantiate injury and treatment. The New York State Workers' Compensation Board has now updated the process of claims submission and is holding the workers' comp payers to the same electronic filing of claims for billing. Enter: the revised CMS-1500.
Goals of the Revised CMS-1500
According to the WCB, the CMS-1500 has three goals:
To improve injured worker access to timely and good care.
To consolidate or eliminate certain medical forms.
To increase provider participation in WC as it is easier to use than the forms it will be replacing, mainly because it relies heavily on the attached medical narrative (providers have commented the current forms are too time consuming).
What is the CMS-1500 Replacing?
The CMS-1500 will ultimately replace the C-4, EC-4, C-4.1, C-4.2, EC4.2, C-4AMR, EC-4AMR, EC-4 NARR, OT/PT-4, EOT/PT-4, PS-4 and C-5 forms.
The CMS-1500 will not replace the Doctor’s Report of MMI/Permanent Impairment Report, C4.3 is not changing.
When Do I Need to Start Using The CMS-1500?
During Phase One, which is the current phase, the forms listed above may still be submitted and considered valid. During this phase, CMS-1500s may be submitted directly to the Board with all fields completed and sufficient attached medical narratives.
Phase Two will be mandatory as of October 1, 2021 and Phase Three will be mandatory in the first quarter of 2022. Find out more about the details of Phase One, Two and Three here.
During Phase Three, CMS-1500s must be submitted through a Board Certified clearinghouse/XML submission partner.
Six Things You Need to Know About the CMS-1500
Here are the six most important things you need to know about the CMS-1500:
Most areas of the CMS-1500 are the same or easily translated from the current forms. (There are sample forms with easy to follow conversion steps available for viewing on the Board.)
All CMS-1500 forms must be submitted with an attached medical narrative report. There is no work around or exceptions to this rule. If a CMS-1500 is submitted through a clearinghouse without a narrative it will automatically be denied.
The format for the attached medical narrative is very specific. The Work Status, Temporary Impairment and Causation/Opinion needs to be addressed at the top of the narrative.
All CMS-1500 submissions must be signed. E-signatures are acceptable.
You can visit wcb.ny.gov/CMS-1500 to explore additional CMS-1500 resources.
Any questions can be emailed to CMS1500@wcb.ny.gov.
To learn more about the revised CMS-1500, here’s a 2019 webinar from the WCB.
NY WC MTG: Go Deeper
Here at Viscardi, we’re passionate about simplifying and humanizing Workers Comp’ and the NY WC MTG (we know it can be a little overwhelming, especially if you’re just getting up to speed). With that in mind, we created three comprehensive, easy to understand NY WC MTG trainings—one for Claims Management Leaders, HR Managers and Account Managers and Sales Executives.
If you need to understand the Treatment Guidelines in more detail, you can learn more about our trainings here.